It's no secret that spending extended periods in space takes a toll on the human body. For years, NASA and other space agencies have been researching the effects of microgravity on humans, animals, and plants aboard the International Space Station (ISS). So far, the research has shown that being in space for long periods leads to muscle atrophy, bone density loss, changes in vision, gene expression, and psychological issues. Knowing these effects and how to mitigate them is essential given our future space exploration goals, which include long-duration missions to the Moon, Mars, and beyond.
However, according to a recent experiment led by researchers at Johns Hopkins University and supported by NASA's Johnson Space Center, it appears that heart tissues "really don't fare well in space" either. The experiment consisted of 48 samples of human bioengineered heart tissue being sent to the ISS for 30 days. As they indicate in their paper, the experiment demonstrates that exposure to microgravity weakens heart tissue and weakens its ability to maintain rhythmic beats. These results indicate that additional measures must be taken to ensure humans can maintain their cardiovascular health in space.
The study was led by Deok-Ho Kim and his colleagues from the Department of Biomedical Engineering at Johns Hopkins University (BME-JHU) and the JHU Center for Microphysiological Systems. They were joined by researchers from UC Boulder's Ann and HJ Smead Department of Aerospace Engineering Sciences, the Institute for Stem Cell & Regenerative Medicine (ISCRM) and the Center for Cardiovascular Biology at the University of Washington, the Stanford Institute for Stem Cell & Regenerative Medicine, BioServe Space Technologies, and NASA's Johnson Space Center. The paper that details their findings was published yesterday (September 23rd) in the *Proceedings of the National Academy of Sciences*.
Previous research has shown that astronauts returning to Earth from the ISS suffer from a myriad of health effects consistent with certain age-related conditions, including reduced heart muscle function and irregular heartbeats (arrhythmias), most of which will dissipate over time. However, none of this research has addressed what happens at the cellular and molecular level. To learn more about these effects and how to mitigate them, Kim and his colleagues sent an automated "heart-on-a-chip" platform to the ISS for study.
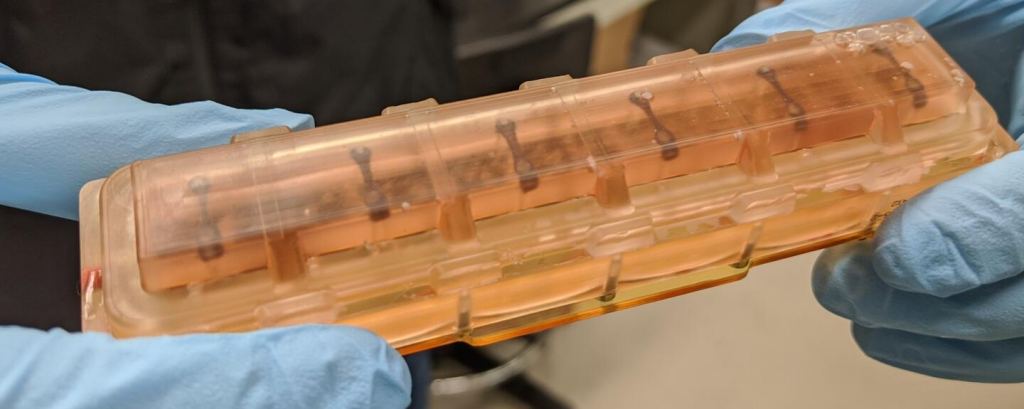
To create this payload, the team relied on human-induced pluripotent stem cells (iPSCs), which can become many types of cells, to produce cardiomyocytes (heart muscle cells). These resulting tissues were placed in a miniaturized bioengineered tissue chip designed to mimic the environment of an adult human heart. The chips would then collect data on how the tissues would rhythmically contract, imitating how the heart beats. One set of biochips was launched aboard the SpaceX CRS-20 mission to the ISS in March 2020, while another was kept on Earth as a control group.
Once on the ISS, astronaut Jessica Meir tended the experiment, changing the liquid nutrients surrounding the tissues once each week while preserving tissue samples at specific intervals so gene readout and imaging analyses could be conducted upon their return to Earth. Meanwhile, the experiment sent real-time data back to Earth every 30 minutes (for 10 seconds at a time) on the tissue samples' contractions and any irregular beating patterns (arrhythmias).
"An incredible amount of cutting-edge technology in the areas of stem cell and tissue engineering, biosensors and bioelectronics, and microfabrication went into ensuring the viability of these tissues in space," said Kim in a recent Hub news release.
When the tissue chambers returned to Earth, he and his colleagues continued to maintain and collect data from the samples to see if there was any change in their abilities to contract. In addition to losing strength, the muscle tissues developed arrhythmias, consistent with age-related heart conditions. In a healthy human heart, the time between beats is about a second, whereas the tissue samples lasted nearly five times as long - though they returned to nearly normal once returned to Earth.
The team further found that the tissue cell's protein bundles that help them contract (sarcomeres) were shorter and more disordered than those of the control group, another symptom of heart disease. What's more, the mitochondria in the tissue samples grew larger and rounder and lost the characteristic folds that help them produce and use energy. Lastly, the gene readout in the tissues showed increased gene production related to inflammation and an imbalance of free radicals and antioxidants (oxidative stress).
This is not only consistent with age-related heart disease but also consistently demonstrated in astronauts' post-flight checks. The team says these findings expand our scientific knowledge of microgravity's potential effects on human health in space and could also advance the study of heart muscle aging and therapeutics on Earth. In 2023, Kim's lab followed up on this experiment by sending a second batch of tissue samples to the ISS to test drugs that could help protect heart muscles from the effects of microgravity and help people maintain heart function as they age.
Meanwhile, the team continues to improve its tissue-on-a-chip system and has teamed up with NASA's Space Radiation Laboratory to study the effects of space radiation on heart muscles. These tests will assess the threat solar and cosmic rays pose to cardiovascular health beyond Low Earth Orbit (LEO), where Earth's magnetic field protects against most space radiation.
*Further Reading: John Hopkins University*, PNAS
 Universe Today
Universe Today